Diabetic Foot Care
When Is Amputation Necessary?
The goals of treatment of diabetic foot problems are not only to save the life and limb, but also to get the patient healed and moving about as soon as possible. If vascular surgery cannot improve blood flow and podiatric surgery cannot restore function, amputation may be the only solution that gets the patient walking again. Amputation may involve one or two toes, part of the foot, or part of the leg. It is selected on the basis of the patients’ condition and level of predicted healing. A return to normal life is especially possible today because of advances in prosthetics.
If you have had a lower extremity amputation due to diabetes or vascular problems, you can dramatically reduce the chances of amputation of the sound foot/leg by following a preventative diabetic foot care program.
General Guidelines for Foot Care:
- Take care of your diabetes by keeping blood glucose in the target range
- Be more active and include exercise in your daily routine
- Don’t sit or lay with crossed legs or ankles
- Don’t smoke; Smoking restricts blood flow in your feet
- Don’t drink excessive alcohol
- Inspect your feet daily
Amputation Types:
If you have a transtibial (below-knee) amputation, never sit or sleep with:
- A pillow under your knee, as this will lead to a contracture (inability to straighten the knee).
If you have a transfemoral (above-knee) amputation, DO NOT sleep with:
- Your limb resting on a pillow, as this promotes a hip flexion contracture (inability to completely straighten your hip)
- A pillow between your legs, as this lengthens the inner thigh muscle that helps you keep your legs together when you walk, and shortens the outer thigh muscles so that you walk and stand with your feet apart.
- Do stretching exercises daily to make sure that you can straighten your knee and hip; this makes walking, and even lying in bed, more comfortable.
Skincare:
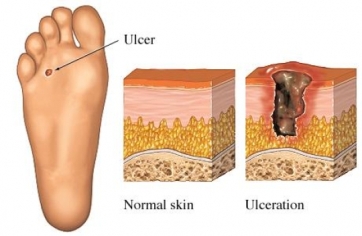
- Infections and ulcers (sores) that don’t heal. Because of poor circulation in the feet, cuts or blisters can easily turn into ulcers that become infected and won’t heal. This is a common-and serious-complication of diabetes and can lead to a loss of your foot, your leg, or your life. An ulcer is a sore in the skin that may go all the way to the bone.
- Wash your limb with mild soap and water every day (more often if you sweat heavily) and pat it dry with a soft towel. Be patient and allow it to dry completely. If this is not done, you will be at risk for fungal growth that could lead to infection or abrasion. A nurse or podiatrist should trim the toenails. Never cut or use over-the-counter removal products for corns or calluses; see your podiatrist instead.
- Never go barefoot! Keep shoes next to the bed and get in the habit of automatically slipping them on as soon as you stand up.
- Protect your feet by wearing socks and shoes at all times.
- It also important to protect your feet from hot and cold. Always wear shoes at the beach or on hot pavement. NEVER put your feet into hot water. Test water before putting your feet in just as you would before bathing a baby. Also do not use a hot water bottle, heating pad, or electric blanket on your foot. You could burn the skin without even realizing it.
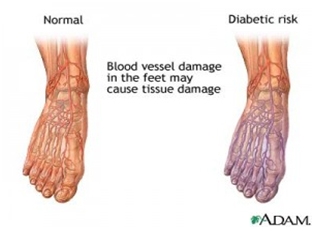
- Observe for changes in circulation. Pay attention to the colour of your toes. If they turn red, pink, or purplish when your legs hang down while sitting, poor circulation may be a problem. Check your limb for red pressure patches that last more than a few minutes after you remove your prosthesis; these may be a sign that the socket needs checking. If left untended, these red patches may result in skin breakdown.
- If you are having a fit problem with your socket, causing skin breakdown, go to your prosthetist for an adjustment. If the breakdown is infected, you will need to go to your physician as well. Stop using the prosthesis; have crutches and a wheelchair for backup.
Diabetic shoes:
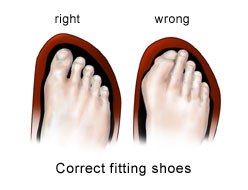
People with diabetes and particularly diabetic neuropathy, need to pay special attention to the style and fit of the shoes they wear and should wear comfortable shoes that fit correctly and do not create focused pressure points. Weight-bearing forces should be evenly distributed across the bottom of the foot.
Insoles should be made of a cushioning fiber or gel and should be replaced when they become compressed. Special diabetic shoes may be recommended in some cases, but are not always necessary. Get in the habit of checking inside the shoe before putting it on to make sure the lining is smooth and that there are no objects inside.
Centre Harika offers a line of shoes and inserts that are made from breathable materials and are designed to cushion while providing extra support to the ankle, arch and heel. By evenly distributing body weight across the foot, these shoes help prevent painful pressure points, blisters and sores from developing. The extra depth shoe design allows room for special foot orthoses.